Decades ago, diabetes affected around 5 million Americans. Diabetic retinopathy was responsible for about 20 percent of new cases of blindness between the ages of 45 and 74. Half of all patients diagnosed with severe forms of diabetic retinopathy went blind within 5 years. At that time, researchers did not recognize the need for persistent blood sugar control to help prevent the complications that arose from diabetes. Diabetic retinopathy did not have effective treatments years ago, resulting in patients who experienced loss of their vision and patients losing independence.
Treatment of diabetic retinopathy is typically determined after using fluorescein angiography (FA) to provide images of the vessels in the back of the eye. These images accurately guide your doctor to the correct treatment plan for you. A FA can identify the location of blood vessel leakage caused by proliferative diabetic retinopathy.
The FA is a diagnostic test where a water-soluble, vegetable-based dye is injected into a vein normally in the hand or arm, and is seen with special filters on a camera that “light up” and map out the diabetic retinopathy your doctor is following. Some doctors repeat this test after series of treatments to assess the improvement or progression of diabetic retinopathy.
Treatments for diabetic retinopathy range from intraocular injections of medication, laser treatments to surgery for severe cases. To understand why your retina specialist chooses specific treatment options, we need to delve into the science happening in the eyes during different stages of the disease.
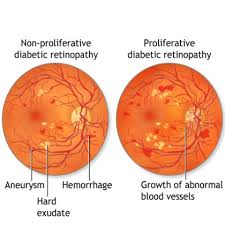
The appearance of diabetic retinopathy is associated with a protein called vascular endothelial growth factor (VEGF) in the retina. VEGF stimulates the production of new blood vessels in the retina to bring more oxygen to the tissue because retinal blood circulation is inadequate due to diabetes.
Unfortunately, these tiny new blood vessels that form in the retina in response to VEGF are fragile and increase in number, leading to additional fluid leakage, bleeding and scarring in the retina and progressive vision loss. Injections are usually an Anti-VEGF inhibitor that helps to reduce the number of these abnormal vessels and to help stop the growth of these vessels that cause macular swelling (edema).
Diabetic macular edema (DME) is a swelling or thickening of the macula. The macula is the small area in the center of the retina, which allows us to see fine details clearly. DME is caused by fluid leaking from small retinal blood vessels damaged by diabetes, and this causes blurred vision. It is the most common cause of visual loss in diabetes. Vision loss can range from mild to severe, but even in the worst cases, peripheral vision continues to function. The main goal of treatment is to prevent further loss of vision, but improvement in vision is possible.
Ozurdex, a FDA-approved implant for diabetic macular edema treatment, slowly releases a sustained dose of dexamethasone (steroid) to the retina after it is injected into the back of the eye. In September 2014, Ozurdex received approval for all patients with diabetic macular edema allowing patients and doctors another option to help reduce the swelling in the back of the eye.
Conventional laser treatment for DME uses a continuous-wave laser to create numerous small burns in the retina. While conventional laser is an effective treatment, the retinal burns, resulting in permanent and often progressive retinal scarring, and can cause visual loss.

In contrast to conventional laser treatment, MicroPulse laser therapy (MPLT) has been proven effective without producing laser burns. MPLT chops the continuous-wave laser beam into a train of tiny, repetitive, low energy pulses separated by a brief rest period in between. This “micropulsing” allows the retina to cool between laser pulses, preventing burns and retinal damage. With MPLT, risks are reduced or eliminated, with less pain and discomfort than conventional laser treatment; and therefore, can be repeated as needed without harm to your vision.
Some people who have proliferative diabetic retinopathy, bleeding into the vitreous (vitreous hemorrhage) makes laser treatments impossible because the blood obscures the surgeon’s view of the retina. When you have decreased vision due to blood in the eye, the doctor also has a very poor view of the back of your eye.
If the vitreous hemorrhage fails to clear or is not resolving within a few weeks, a vitrectomy may be performed to mechanically remove the hemorrhage. A possible laser procedure is performed either at the time of the vitrectomy or shortly thereafter.
Retinal bleeding and vitreous hemorrhage also can cause scar tissue to form on the retina. These bands of scar tissue can shrink and if attached to the retina, may cause the retina to pull away and create traction on the retina. This traction may lead to retinal tears or possible retinal detachments.
 A tractional retinal detachment is part of the many complications of PDR and is shrinking scar tissue that tugs at the retina. If you experience a tractional detached retina, you will be scheduled promptly for a procedure to reattach the retina. Some guidelines show that type 2 diabetics in particular can reduce their chance of severe vision loss and the need for vitrectomy surgery by about 50 percent when proliferative diabetic retinopathy is treated before it reaches a high-risk stage.
A tractional retinal detachment is part of the many complications of PDR and is shrinking scar tissue that tugs at the retina. If you experience a tractional detached retina, you will be scheduled promptly for a procedure to reattach the retina. Some guidelines show that type 2 diabetics in particular can reduce their chance of severe vision loss and the need for vitrectomy surgery by about 50 percent when proliferative diabetic retinopathy is treated before it reaches a high-risk stage.
The most effective diabetic retinopathy programs will take a holistic approach, focusing on patient education, behavior change, and effective disease management strategies in addition to the provision of annual dilated exams and high quality, affordable treatment, when required. Increased cooperation between the diabetes care and ophthalmic communities is essential to preventing the impending epidemic of vision loss due to diabetic retinopathy and the other possible pathologies that may occur.
Roger T. Adler, MD is Bond Eye Associates’ Retina Specialist. He is accepting new patients in both of their locations: Peoria, and Pekin, IL. Please call 309-692-2020 or click here to schedule an appointment.