This is the reaction we get from many of our patients when they are told they need an injection in their eye to save their vision. The thought of a needle in your eye is not a pleasant thought. Surprisingly, most patients after their first treatment often tell the technician and doctor that the treatment was not as bad as they had anticipated. With proper education and explanation, we find patients are much more comfortable receiving the recommended treatment for their diagnosis. This article explains the step by step process our retinal specialist uses to perform an injection.


The day of the injection, the patient will present to the office for a dilated exam and imaging. The technician will focus on the eye that is receiving the treatment at that visit. Once the patient is dilated, the patient will be brought into an exam room where the process of the injection begins. The technician will start off by putting several numbing drops into the eye receiving treatment. While the numbing process is taking place, the technician will prepare the necessary items that must be present for the injection to take place. Once the patient is numbed with topical numbing drops and the procedure is explained, the patient is reclined in the exam chair and the physician then gives the patient an injection of 2% lidocaine at the injection site which is used for additional numbing. The doctor will then clean around the eyelids and lashes of the injection eye with a betadine swab. The patient is instructed to avoid touching their eye or anywhere close to the sterile injection site during the procedure. The doctor will then place a sterile speculum in the eye to help keep the eye open during the injection. While the doctor is prepping the medication, the technician will put drops of Betadine in the injection eye to kill any bacteria prior to injection. The physician will then administer the drug by penetrating the eyeball and pushing the medication into the jelly-like substance at the back of the eye called the vitreous. After the needle is removed, a sterile cotton tipped applicator is placed on the site to prevent reflux. The technician will then instill another drop of betadine on the injection site to prevent infection. Once the injection is completed, the doctor will remove the speculum and clean around the patient’s eye with a sterile eye pad making sure that most of the betadine is wiped clean from the face.
The technician will then go over, in detail, all post procedure instructions. The patient will also be given a post op instruction sheet to refer to once they are home. Instructions include:
- no makeup (if applicable) for 3 days following the injection
- no eye drops for 3 days following the injection except preservative free artificial tears
- leave the betadine on the eye for 24 hours post injection
- use clean tissues when pat drying any excess fluid.
This sheet will also include things that they may experience, post injection, that are normal and abnormal. Patients may experience post procedural irritation, this is normal due to the betadine causing irritation. In addition, they may experience bloody discharge on a clean tissue after the procedure. The blood will subside within hours after injection. If the patient experiences extreme pain, decreasing vision, or sudden vision loss, the patient is instructed to call our office immediately.
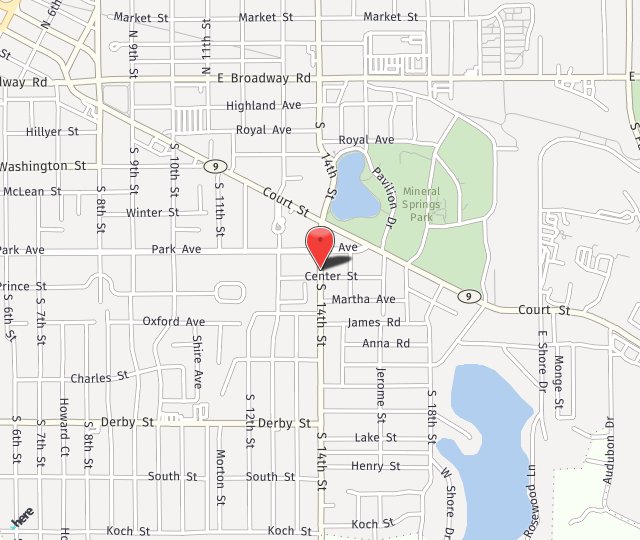
Click here or Call toll free at 800-243-2020 to schedule your yearly health vision exam with confidence knowing that they have been a trusted, locally owned, medical practice for over 40 years. They are accepting new patients in both of their locations: Peoria and Pekin, IL.