Many diabetics, particularly those with poor diabetic control, have damaged the blood vessels in the retina. The retina is the tissue lining the back of the eye that detects light and allows us to see with crisp, clear vision. This condition is called diabetic retinopathy and will affect 8 out of 10 patients who have had diabetes for 10 years or more.
I have seen very few patients with diabetes over 30 years that are lucky enough not to have developed the disease. It is safe to say that most will develop the disease at some point in their lives and I tell all my patients to expect the diabetic retinopathy to develop. Not that it will, but all diabetic patients should expect it. Why? If you expect the disease to develop, you are more likely to have regular dilated vision exams. Many people with diabetes are not aware of their vision condition or that they may require treatment. If left unmanaged and untreated, diabetic retinopathy may slowly or suddenly affect their vision and lead to blindness.
Diabetic retinopathy is where fluid leaks out of the tiny damaged blood vessels in the back of the eye. The fluid accumulates in the macula, the central part of the retina which is responsible for seeing fine details and is responsible for our central vision. This leads to swelling (edema) of the macula and causes blurred vision. Eventually, patients with macular edema can develop a poor central vision and be unable to read or even drive, however, the vision to the side usually remains normal.
There are 2 types of diabetic retinopathy: background diabetic retinopathy and proliferative diabetic retinopathy. Background diabetic retinopathy or also more commonly called non-proliferative diabetic retinopathy (NPDR), is normally staged by your Ophthalmologist as stable, mild, moderate, or severe. The doctor stages your condition depending on the visible damage seen to the small blood vessels and the amount of macular edema noted during your exam. NPDR accounts for approximately 80% of all diabetic retinopathy cases and is the most common form.
Proliferative diabetic retinopathy (PDR) is when your doctor sees severe small retinal vessel damage, and reduced oxygenation of the retina. This reduced oxygenation causes the retina to react by growing abnormal blood vessels (neovascularization). These abnormal blood vessels are fragile and can bleed and pull on the retina as they grow. Bleeding into the vitreous cavity of the eye (vitreous hemorrhage) can result in sudden and sometimes severe loss of vision. This type of hemorrhage is painless and, early on, may look like cobweb-like floaters. The pulling on the retina that is caused by the abnormal vessels may also cause a tractional retinal detachment.
People with diabetic retinopathy whose sight is at risk can be treated to prevent visual impairment and blindness. Contrary to beliefs in the past, in most cases treatment can restore vision that has already been lost. However, most patients who develop diabetic retinopathy have no symptoms until the very late (severe) stages. In which time may be too late for effective treatment to regain viable vision. Therefore screening and early intervention are critical. It is recommended to have a yearly dilated exam with your Ophthalmologist if you are not currently being treated.

Diabetic retinopathy left untreated, or poor compliance with treatment, can cause advanced pathologies directly related to diabetic retinopathy. A vitreous hemorrhage is when the damaged blood vessels in the back of the eye (retina) begin to fill the eye with blood causing sudden decreased vision. Another pathology is an aggressive type of Glaucoma that can develop rapidly. There are many types of Glaucoma, but this particular type can cause a blind, painful eye. Patients with Diabetes are at a higher risk for developing cataracts earlier in life. These are just some of the subsequent problems and complications that can arise from diabetic retinopathy if left untreated.
There is good evidence that making appropriate lifestyle changes can contain or even reverse the usual form of the disease. The relevant lifestyle changes involve a sensible lower carbohydrate diet, increased exercise, control of high blood pressure, control of high blood sugar and cholesterol. This is the main health care approach that can result in lowering the prevalence of diabetes and the possible diabetic manifestations.
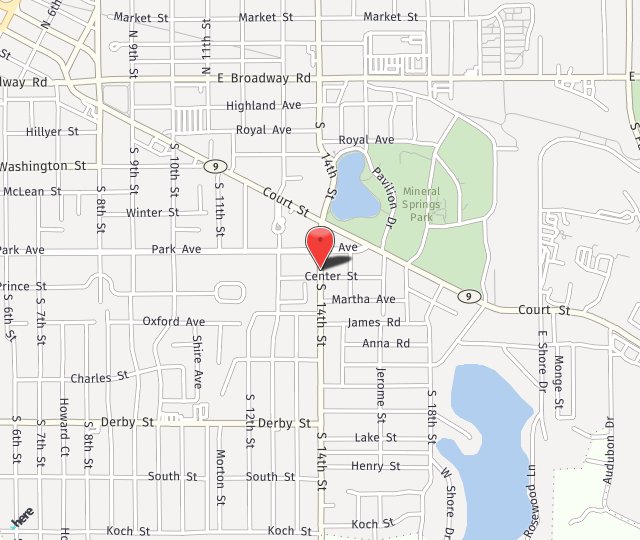
Roger T. Adler, MD is Bond Eye Associates’ Retina Specialist. He is accepting new patients in both of their locations: Peoria and Pekin, IL. Please call 309-692-2020 to schedule an appointment.